Recent Physician Services Agreement (PSA) updates have brought significant changes for FHO and FHN physicians. In addition to the upcoming transition of the fee-for-service hard cap to an individual level, the Ministry has discontinued preventive care bonuses across three categories,. These changes have been an ongoing topic of discussion within the medical community, and in response, the OMA has introduced a new acuity modifier payment structure. This aims to repurpose the funds and continue providing compensation for the care of complex patients, mitigating the impact of these recent changes.
To help physicians understand the details of this update, mainly how it affects existing capitation and its relationship with patient diagnoses, we will explore the different components of the acuity modifier payment, review relevant diagnostic codes and address common questions from doctors regarding the new update.
The New Acuity Modifier Update
With the partial removal of preventive care categories, physicians may be left wondering how they will recoup lost revenue. Effective April 1, 2024, physicians in the FHN and FHO models will receive an additional payment based on the acuity of patients enrolled, measured by the Canadian Institute for Health Information’s Population Grouping Method.
Each patient in Ontario is assigned a risk score based on:
- Age
- Sex
- Activities of daily living (ADL) and
- Health condition(s) using the CIHI POP Grouper.
Patients within each age-sex group are arranged in increasing order of their risk scores and categorized into five bands.
Understanding The Five Acuity Bands
One of the main highlights of the new acuity payment modifier update is the creation of bands.
These bands indicate the acuity or level of complexity for patients, ranging from one (least acute) to five (most acute). It’s worth noting that “acuity” encompasses acute and chronic conditions affecting patients’ demand for healthcare resources.
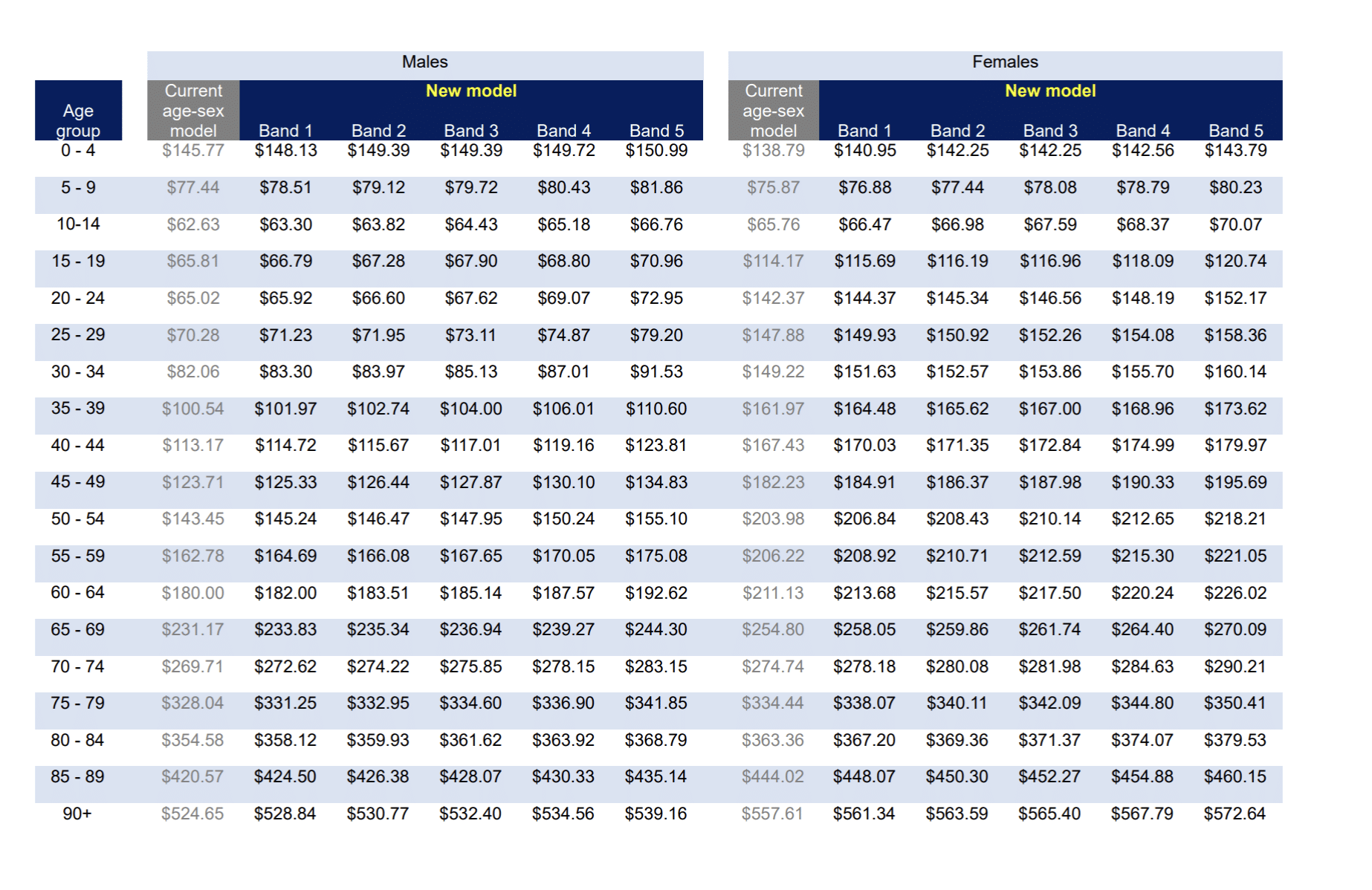
The OMA table below illustrates the new annual capitation rates for males and females under the FHO and FHN payment models across the five bands:
New Annual FHO Capitation Rates
New Annual FHN Capitation Rates
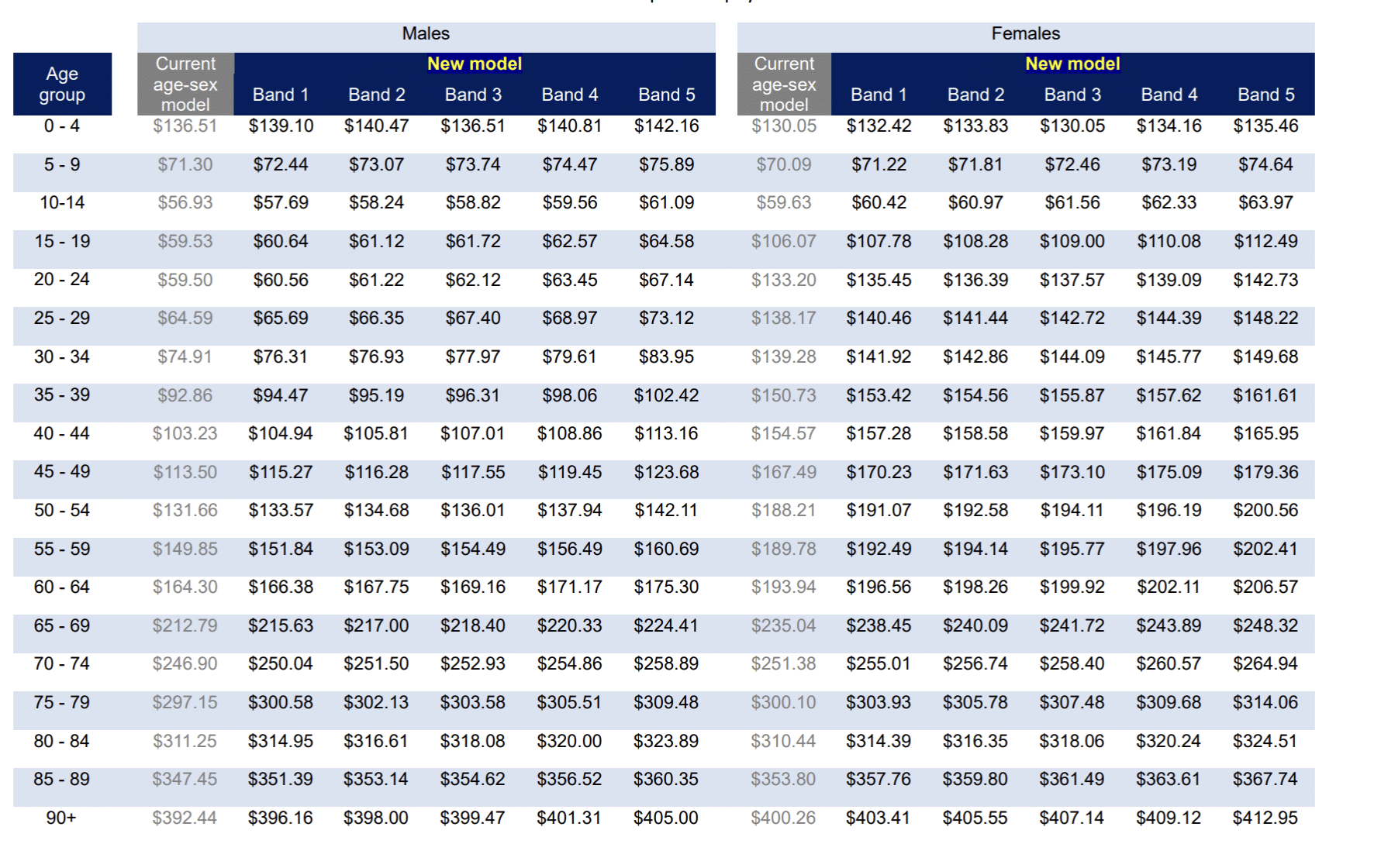
By categorizing patients into bands based on complexity permutations, we create five tiers, each comprising around 1.1 million potential complexities. The lower bands contain non-users and acute disorders, while higher bands house complex and chronic cases requiring extensive healthcare resources, leading to higher acuity payments.
Good news! As a physician, you don’t need to worry about determining what band a patient falls under; that is entirely the Ministry’s responsibility. Doctors should focus on using precise diagnostic codes in their patient visits to ensure proper assignment to bands and maximize patient capitation.
The Acuity Modifier Relationship to Diagnostic Codes
It is worth mentioning that the CIHI Population Grouping Method assigns patients to various health profiles based on their diagnoses rather than the nature of the visit. This underscores the importance of all doctors prioritizing the use of accurate diagnostic codes in their OHIP claims.
Given the significance of precise diagnoses, it’s recommended to avoid utilizing generic diagnostic codes like ‘799—Non-specific Abnormal Findings: Other ill-defined conditions’ during patient consultations. Doing so may impact patient classification into bands and subsequent payments.
Opting for more specific diagnostic codes, such as code 493 for asthma rather than 786, will enhance the precision of your patient visits and ensure more accurate capitation payments.
Acuity Modifier Payment Schedule
As we explore the latest updates from the Ministry, it is important to note that all FHN and FHO physicians who practiced during the fiscal year 2022/2023 will receive a new one-time acuity payment disbursed as a lump sum for the fiscal year 2024/2025. You would have already received this payment in the May 2024 remittance advice (RA) alongside your regular capitation amount.
This one-time payment for the entire fiscal year 2024/2025 will be listed under the accounting transaction ‘BASE RATE ACUITY PAYMENT’.
Physicians who commenced practice in the fiscal year 2023/2024 or will begin practicing in fiscal 2024-2025 will receive their one-time new acuity payment for 2024/2025 in the fall of 2025. This is because the data for physicians who started practising after April 1, 2023, is incomplete to make a one-time interim payment after April 1, 2024. The complete data for these physicians will be available after the summer of 2025, and their interim payment will be made after September 1, 2025. This payment is retroactive for April 1, 2024, and March 31, 2025.
Anticipated interim payment date | Physician cohort | Physician payment | Repurposed fund |
After April 1, 2024 | Started practice prior to April 1, 2023 | One-time interim payment for service provided from April 1, 2024, to March 31, 2025 | Preventive care bonuses |
After June 1, 2025 | Started practice after April 1, 2023 | One-time interim payment for service provided from April 1, 2024, to March 31, 2025 | Preventive care bonuses |
TBD | All physicians | Permanent, ongoing automated monthly payment after April 1, 2025 | Preventive care bonuses and changes to the maximum fee-for-service pooling from groups to individual physicians (hard cap) |
Starting April 1, 2025, acuity payments will be automatically added to the monthly capitation payments for all FHN and FHO physicians, detailed in their monthly remittance advice (RA). Further information will be provided closer to the implementation date.
Frequently Asked Questions
What exactly does the new acuity modifier payment take into consideration?
The system considers fee codes billed by family physicians and any other claims in other settings, such as hospitals and emergency departments. Although OHIP currently only accepts a single diagnosis per claim, a patient’s diagnostic profile is assembled of all a patient’s physician visits, and health-system encounters over many years. For example, data from inpatient and ED visits allow multiple diagnostic codes to be reported simultaneously. Accurate diagnosis reporting with each OHIP claim can help to ensure that patient complexity is properly captured by the methodology.
What is the timeframe for billing data that is being used to group patients into bands?
When assigning patients to complexity bands, the Ministry looks at data going back:
- Five years for chronic conditions (i.e. asthma, cancer, diabetes)
- Two years for acute conditions (i.e. URTIs, UTIs, stitches)
It takes two diagnoses to trigger the acuity modifier to be updated.
Do service codes affect what band a patient is assigned to?
Billing different service codes does not impact a patient’s band assignment. Whether you bill K030, A005, or K013, it does not affect the band to which a patient is ultimately assigned.
Does my roster size affect the new acuity payments?
All roster sizes, including those with fewer than 1000 patients, will receive the new acuity payments. Physicians with more enrolled patients receive higher capitation payments, and the new system further recognizes the acuity of each patient.
What happens when a specialist sees my patient?
If a patient goes to see a specialist and that specialist bills a different diagnosis, it helps the family provider with the acuity modifier. So, if you know a patient is seeing a cardiologist for CHF, you should bill a different diagnosis when that patient comes to see you as their family physician.
As a physician, is there anything I need to do on my part to receive these payments?
It’s important to note that patient assignment to bands is the responsibility of the Ministry, not healthcare professionals. As a physician, your role remains unchanged. You will continue to submit your claims as usual and reflect the patient diagnosis on the claim using accurate diagnosis coding. This process ensures that you can focus on providing the best care for your patients without the added burden of patient assignment.
Key Takeaways
This year has brought significant changes for FHO and FHN physicians, including the partial removal of preventive care bonuses in three categories and the anticipated transition of the fee-for-service hard cap to an individual level. Moving away from broad, nonspecific diagnostic codes and embracing more precise ones during patient visits is a significant change. This practice not only aids the Ministry in categorizing patients more accurately by complexity bands, but also optimizes revenue potential in the long run.
We are here to help.
Looking to streamline your medical billing process? DoctorCare is here to help with a complimentary billing assessment. Our experts will conduct a comprehensive audit of your billings and uncover revenue-maximizing opportunities. Let us alleviate the billing burden, allowing you to dedicate your full attention to providing top-notch patient care.
Contact us today for your free billing assessment!